肋木躯干柔韧性练习
是通过肋木练习,提高躯干肌肉和韧带的伸屈能力,增加胸、腰椎和髋关节活动幅度的一种柔韧性素质的练习方法。利用肋木可做体前屈、体后屈和体侧屈等动作内容的练习。适合老年人练习的动作如:
体前屈背对肋木并腿或分腿站立,上体尽量前屈,贴近两腿,两手从腿侧或两腿中向体后握木杆,身体前移用力,保持腿伸直。
体后屈面对或侧对肋木站立,两手或一手扶木,抬头挺胸展髋,上体尽量后屈,眼看地。
体侧屈侧对肋木分腿站立,一手从头上,一手从体侧扶木,上体尽量向木侧屈,髋、腰部向外侧用力。上述动作见图2—3—12。动作练习中要做有节奏性的屈伸用力,根据个人的柔韧情况,调节站位距离和扶木的高度。
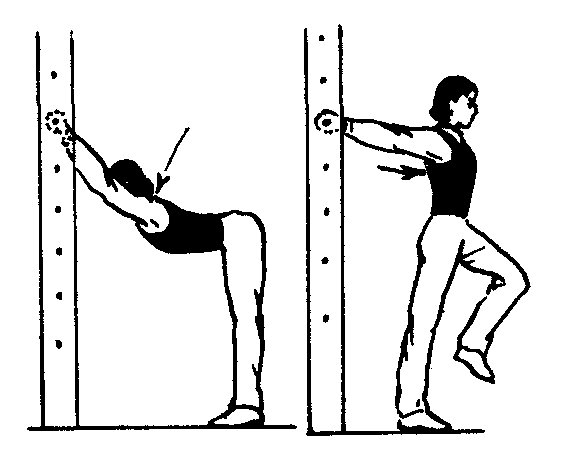
图2—3—12 肋木躯干柔韧性练习